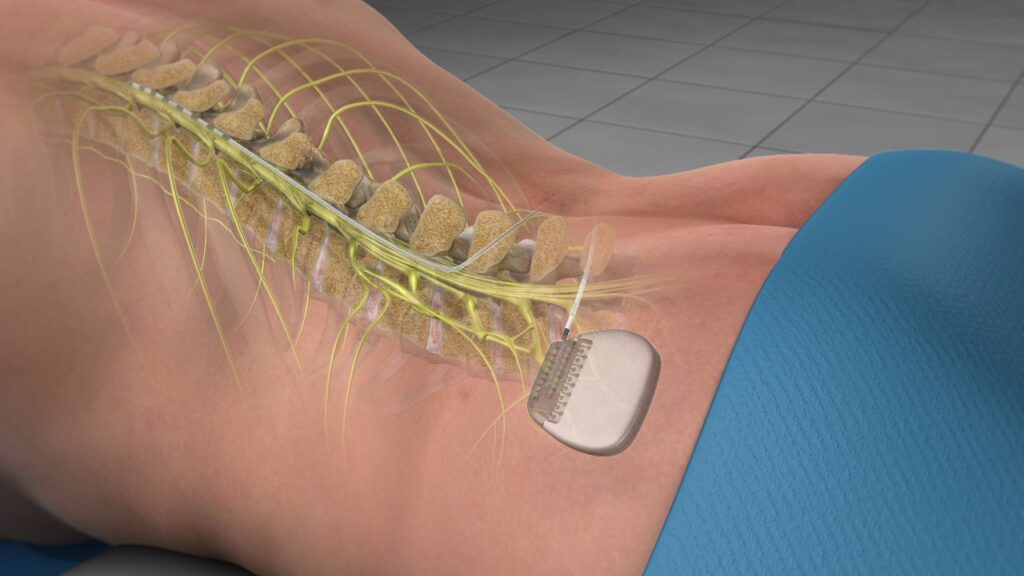
Spinal Cord Stimulators are implanted devices used to relieve the pain signals that are being communicated through the spinal cord. The devices consist of thin wires (electrodes) and a small, pacemaker-like battery pack (the generator). The electrodes are placed between the spinal cord and the vertebrae (the epidural space), and the generator is placed under the skin, usually near the buttocks or abdomen.
The device allows patients to direct mild electrical pulses using a remote control when they feel pain. Pain is reduced because the electrical pulses modify and mask the pain signal from reaching your brain. Stimulation does not eliminate the source of pain, it simply changes the way the brain perceives it. Spinal cord stimulation (SCS) is used most often after nonsurgical pain treatment options have failed to provide sufficient relief.
The first step in the process is an evaluation of your physical condition, medication regime, and pain history to see if your pain management goals are appropriate for Spinal Cord Stimulation.
You may be a good candidate for SCS if:
- Prior conservative therapies have failed.
- Additional surgery would not offer a benefit.
- You do not want to undergo further surgery due to the risks or the long recovery.
- You do not have untreated depression or a drug addiction.
- You have no medical conditions that would prevent you from undergoing the procedure
Patients selected for SCS usually have had chronic debilitating pain for more than 6 months. SCS can help lessen chronic pain caused by:
- Chronic leg (sciatica) or arm pain: ongoing, persistent pain caused by arthritis, spinal stenosis, or by nerve damage.
- Diabetic neuropathy: A type of nerve damage that can cause burning or stabbing pain, often in the legs or feet.
- Failed back surgery syndrome: failure of one or more surgeries to relieve persistent arm or leg pain, but not a technical failure of the original procedure.
- Complex regional pain syndrome: a progressive disease in which patients feel constant, chronic burning pain, typically in the foot or hand.
- Arachnoiditis: painful inflammation and scarring of the protective lining of the spinal nerves.
- Other: stump pain, peripheral vascular disease, multiple sclerosis, or spinal cord injury.
If your doctor feels that you are a good candidate for Spinal Cord Stimulation, you would move onto the Trial stage. Spinal cord stimulators require two procedures to test and implant the device: the trial and the implantation.
Trial "The Test Drive"
Trial stimulation is a “test drive” to determine if an SCS will work for the type, location, and severity of your pain. It is typically performed in the office.
A local anesthetic is given to numb the area in the lower back. Using X-ray fluoroscopy, a hollow needle is inserted through the skin into the epidural space between the bone and spinal cord. The trial lead is inserted and positioned over specific nerves. The wires are attached to an external generator worn on a belt.
You will be sent home with instructions on how to use the trial stimulator and care for your incision site. Keep a written log of the stimulation settings during different activities and the level of pain relief. After 4 to 7 days, you will return to the doctor’s office to discuss permanently implanting the stimulator or removing the trial leads.
The amount of pain relief varies for each person. The goal for SCS is a minimum of 50 reduction in pain. However, even a small amount of pain reduction can be significant if it helps you perform daily activities and reduces the amount of pain medication you take.
Implantation Procedure
If the trial was successful and you experienced a significant improvement in pain, surgery can be scheduled to implant the SCS device in your body.
This is usually done by making a small incision in the back and another near the waist. The electrode leads are inserted with the aid of fluoroscopy (a type of X-ray). The leads are placed through the incision on the back to the space behind the spinal cord and secured with sutures. Once the lead electrodes are in place, the wire is passed under the skin from the spine to the waist and connected to a small battery powered generator. The generator is placed under the skin at the waist incision. The surgeon will test the system, then close the incisions.
This is a minimally-invasive surgical procedure. Most patients are discharged the same day or possibly the following morning, depending on your medical history.
What happens after implantation?
The pulse generator will be programmed after implantation. Once the SCS has been programmed, you will receive instructions for regulating the stimulation by controlling the strength and the duration of each stimulation period. Your doctor may alter the pulse width, amplitude, and frequencies on follow-up visits if necessary.
The pulse generator has programmable settings:
- Frequency (rate): number of times stimulation is delivered per second. Too few pulses results in no sensation. Too many results in a washboard or bumpy effect.
- Pulse width: the area the stimulation will cover.
- Pulse amplitude: determines threshold of perception to pain.
The handheld programmer gives you the ability to turn the stimulator on and off, select different programs, and adjust the intensity of the stimulation. You may be provided with a variety of programs to help you achieve the most pain relief depending on the time of day, or activities you are engaging in. You may use your spinal cord stimulator around the clock if necessary.
In most cases, the stimulator is barely visible underneath the skin.
What are the risks?
All surgeries carry some risks, but serious side effects and complications from SCS implantation are uncommon. Most commonly, patients may experience some pain where the wires and stimulator were inserted. Your doctor can prescribe pain relief for a few days. Other possible complications include infection, bleeding, nerve injury, spinal cord injury, dural puncture or tear, and migration or breakage of the wire.
In rare cases, you may need additional surgery to address movement of the lead, breakage of the lead or extension wire, or mechanical failure of the device. In some cases, scar tissue develops around the electrode and can make the stimulation less effective. Bottom line, SCS therapy is reversible. If a patient decides at any time to discontinue treatment due to infection or failure to relieve pain, the electrode wires and generator can all be removed.
Studies of spinal cord stimulation show long-term relief in 50 to 80% of patients suffering from chronic pain. One study reports that 24% of patients were able to return to work or housework with stimulation alone or with the addition of occasional oral pain medication.
Spinal cord stimulation is a safe procedure that has been used for decades, and is being utilized for an increasing number of conditions. Spinal cord stimulation can improve the overall quality of your life, and reduce the need for pain medicines. If you are experiencing chronic, persistent pain, and other treatments haven’t given you adequate relief, talk to your physician about referring you to a Pain Management doctor like Dr. Smith for spinal cord stimulation.
If you’re looking for a Texas pain clinic in San Antonio, give us a call today at (210) 963-7493. If you would like to request an appointment online, you can do so through our convenient online appointment request form.

